The Eating Healthy and Daily Life Activities (EHDLA) Study
Abstract
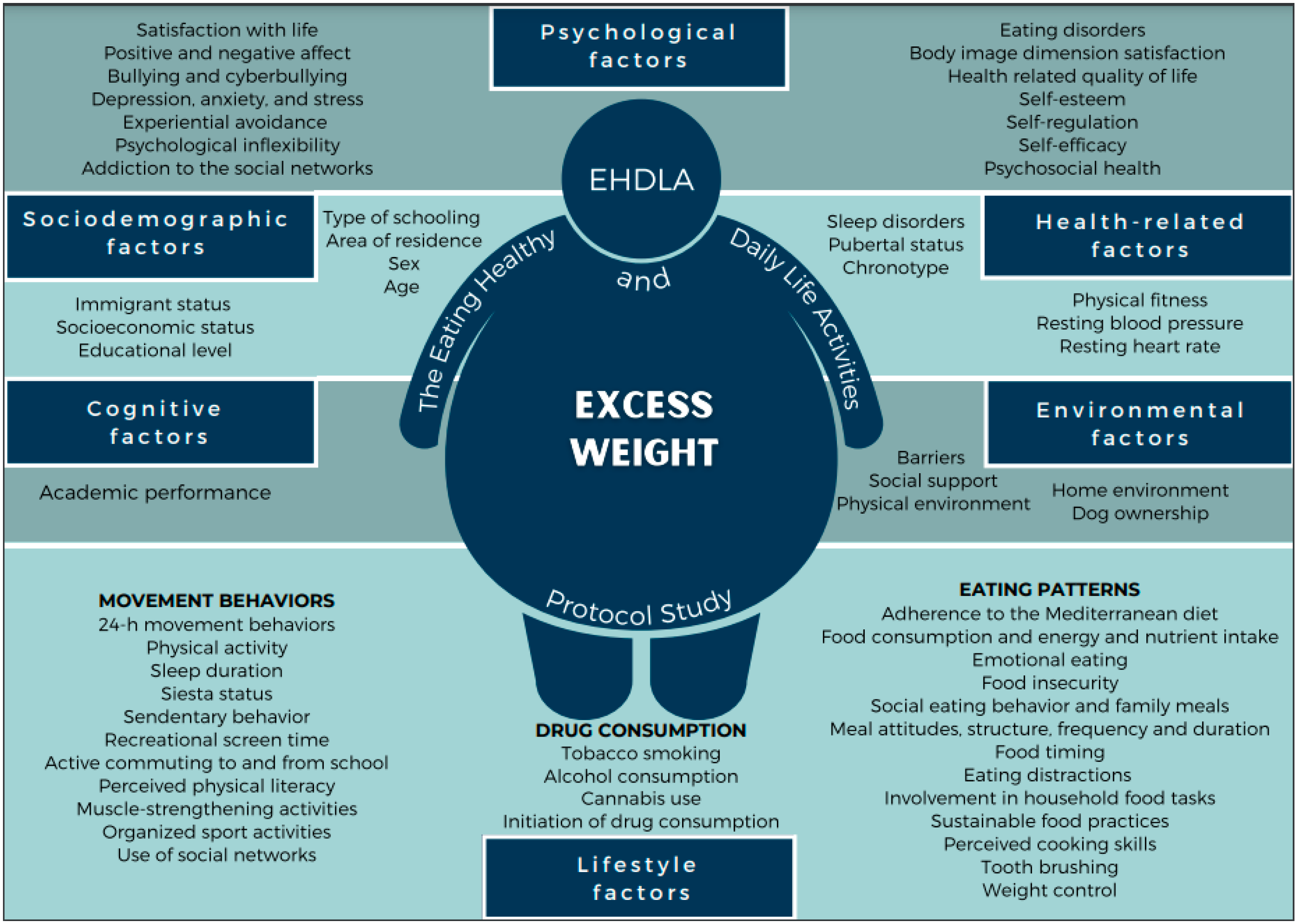
1. Introduction
2. Materials and Methods
2.1. Study Design and Population
2.2. Procedures
2.2.1. Excess Weight Measurements
2.2.2. Sociodemographic Factors
2.2.3. Environmental Factors
2.2.4. Lifestyle Factors
Movement Behaviors
Eating Patterns
Drug Consumption
2.2.5. Health-Related Factors
2.2.6. Cognitive Factors
2.2.7. Psychological Factors
2.3. Statistical Analysis
3. Discussion
4. Conclusions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Abarca-Gómez, L.; Abdeen, Z.A.; Hamid, Z.A.; Abu-Rmeileh, N.M.; Acosta-Cazares, B.; Acuin, C.; Adams, R.J.; Aekplakorn, W.; Afsana, K.; Aguilar-Salinas, C.A.; et al. Worldwide Trends in Body-Mass Index, Underweight, Overweight, and Obesity from 1975 to 2016: A Pooled Analysis of 2416 Population-Based Measurement Studies in 128·9 Million Children, Adolescents, and Adults. Lancet 2017, 390, 2627–2642. [Google Scholar] [CrossRef]
- Rito, A.I.; Buoncristiano, M.; Spinelli, A.; Salanave, B.; Kunešová, M.; Hejgaard, T.; García Solano, M.; Fijałkowska, A.; Sturua, L.; Hyska, J.; et al. Association between Characteristics at Birth, Breastfeeding and Obesity in 22 Countries: The WHO European Childhood Obesity Surveillance Initiative – COSI 2015/2017. Obes. Facts 2019, 12, 226–243. [Google Scholar] [CrossRef] [PubMed]
- Miqueleiz, E.; Lostao, L.; Ortega, P.; Santos, J.M.; Astasio, P.; Regidor, E. Trends in the Prevalence of Childhood Overweight and Obesity According to Socioeconomic Status: Spain, 1987–2007. Eur. J. Clin. Nutr. 2014, 68, 209–214. [Google Scholar] [CrossRef] [PubMed]
- Espín Ríos, M.I.; Pérez Flores, D.; Sánchez Ruíz, J.F.; Salmerón Martínez, D. Prevalencia de obesidad infantil en la Región de Murcia, valorando distintas referencias para el índice de masa corporal. An. Pediatr. 2013, 78, 374–381. [Google Scholar] [CrossRef]
- Kumar, S.; Kelly, A.S. Review of Childhood Obesity: From Epidemiology, Etiology, and Comorbidities to Clinical Assessment and Treatment. Mayo Clin. Proc. 2017, 92, 251–265. [Google Scholar] [CrossRef]
- Umer, A.; Kelley, G.A.; Cottrell, L.E.; Giacobbi, P.; Innes, K.E.; Lilly, C.L. Childhood Obesity and Adult Cardiovascular Disease Risk Factors: A Systematic Review with Meta-Analysis. BMC Public Health 2017, 17, 683. [Google Scholar] [CrossRef]
- World Health Organization; Commission on Ending Childhood Obesity. Report of the Commission on Ending Childhood Obesity; WHO: Geneva, Switzerland, 2016; ISBN 978-92-4-151006-6. [Google Scholar]
- Ministry of Health, Consumer Affairs and Social Welfare. Spanish National Health Survey; Spanish Government: Madrid, Spain, 2018.
- de Bont, J.; Díaz, Y.; Casas, M.; García-Gil, M.; Vrijheid, M.; Duarte-Salles, T. Time Trends and Sociodemographic Factors Associated With Overweight and Obesity in Children and Adolescents in Spain. JAMA Netw. Open 2020, 3, e201171. [Google Scholar] [CrossRef]
- United Nations International Children’s Emergency Fund Spanish Committee. The Rights of Children and Adolescents in the Region of Murcia 2020; United Nations International Children’s Emergency Fund: Murcia, Spain, 2020. [Google Scholar]
- López-Gil, J.F.; López-Benavente, A.; Tárraga López, P.J.; Yuste Lucas, J.L. Sociodemographic Correlates of Obesity among Spanish Schoolchildren: A Cross-Sectional Study. Children 2020, 7, 201. [Google Scholar] [CrossRef]
- Bates, C.R.; Buscemi, J.; Nicholson, L.M.; Cory, M.; Jagpal, A.; Bohnert, A.M. Links between the Organization of the Family Home Environment and Child Obesity: A Systematic Review: Home Organization and Child Obesity. Obes. Rev. 2018, 19, 716–727. [Google Scholar] [CrossRef]
- Dunton, G.F.; Kaplan, J.; Wolch, J.; Jerrett, M.; Reynolds, K.D. Physical Environmental Correlates of Childhood Obesity: A Systematic Review. Obes. Rev. 2009, 10, 393–402. [Google Scholar] [CrossRef]
- Stankov, I.; Olds, T.; Cargo, M. Overweight and Obese Adolescents: What Turns Them off Physical Activity? Int. J. Behav. Nutr. Phys. Act. 2012, 9, 53. [Google Scholar] [CrossRef] [PubMed]
- Poorolajal, J.; Sahraei, F.; Mohamdadi, Y.; Doosti-Irani, A.; Moradi, L. Behavioral Factors Influencing Childhood Obesity: A Systematic Review and Meta-Analysis. Obes. Res. Clin. Pract. 2020, 14, 109–118. [Google Scholar] [CrossRef] [PubMed]
- García-Hermoso, A.; Ramírez-Vélez, R.; García-Alonso, Y.; Alonso-Martínez, A.M.; Izquierdo, M. Association of Cardiorespiratory Fitness Levels During Youth With Health Risk Later in Life: A Systematic Review and Meta-Analysis. JAMA Pediatr. 2020, 174, 952–960. [Google Scholar] [CrossRef]
- García-Hermoso, A.; Ramírez-Campillo, R.; Izquierdo, M. Is Muscular Fitness Associated with Future Health Benefits in Children and Adolescents? A Systematic Review and Meta-Analysis of Longitudinal Studies. Sports Med. 2019, 49, 1079–1094. [Google Scholar] [CrossRef]
- Fatima, Y.; Doi, S.A.R.; Mamun, A.A. Sleep Quality and Obesity in Young Subjects: A Meta-Analysis: Sleep Quality and Obesity. Obes. Rev. 2016, 17, 1154–1166. [Google Scholar] [CrossRef]
- Rankin, J.; Matthews, L.; Cobley, S.; Han, A.; Sanders, R.; Wiltshire, H.D.; Baker, J.S. Psychological Consequences of Childhood Obesity: Psychiatric Comorbidity and Prevention. AHMT 2016, 7, 125–146. [Google Scholar] [CrossRef]
- Dietz, W.H. Periods of Risk in Childhood for the Development of Adult Obesity—What Do We Need to Learn? J. Nutr. 1997, 127, 1884S–1886S. [Google Scholar] [CrossRef]
- Alberga, A.S.; Sigal, R.J.; Goldfield, G.; Prud’ homme, D.; Kenny, G.P. Overweight and Obese Teenagers: Why Is Adolescence a Critical Period? The Critical Period of Adolescence. Pediatr. Obes. 2012, 7, 261–273. [Google Scholar] [CrossRef]
- Psaltopoulou, T.; Tzanninis, S.; Ntanasis-Stathopoulos, I.; Panotopoulos, G.; Kostopoulou, M.; Tzanninis, I.-G.; Tsagianni, A.; Sergentanis, T.N. Prevention and Treatment of Childhood and Adolescent Obesity: A Systematic Review of Meta-Analyses. World J. Pediatr. 2019, 15, 350–381. [Google Scholar] [CrossRef]
- Elvsaas, I.K.Ø.; Giske, L.; Fure, B.; Juvet, L.K. Multicomponent Lifestyle Interventions for Treating Overweight and Obesity in Children and Adolescents: A Systematic Review and Meta-Analyses. J. Obes. 2017, 2017, 1–14. [Google Scholar] [CrossRef]
- Al-Khudairy, L.; Loveman, E.; Colquitt, J.L.; Mead, E.; Johnson, R.E.; Fraser, H.; Olajide, J.; Murphy, M.; Velho, R.M.; O’Malley, C.; et al. Diet, Physical Activity and Behavioural Interventions for the Treatment of Overweight or Obese Adolescents Aged 12 to 17 Years. Cochrane Database Syst. Rev. 2017, 6, 1–341. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization Adolescent Obesity and Related Behaviours: Trends and Inequalities in the Who European Region, 2002–2014: Observations from the Health Behavior in School-Aged Children (HBSC) WHO Collaborative Cross-National Study; World Health Organization, Regional Office for Europe: Copenhagen, Denmark, 2017; ISBN 978-92-890-5240-5.
- de Onis, M. Development of a WHO Growth Reference for School-Aged Children and Adolescents. Bull. World Health Organ. 2007, 85, 660–667. [Google Scholar] [CrossRef] [PubMed]
- Cole, T.J.; Lobstein, T. Extended International (IOTF) Body Mass Index Cut-Offs for Thinness, Overweight and Obesity: Extended International BMI Cut-Offs. Pediatr. Obes. 2012, 7, 284–294. [Google Scholar] [CrossRef] [PubMed]
- Browning, L.M.; Hsieh, S.D.; Ashwell, M. A Systematic Review of Waist-to-Height Ratio as a Screening Tool for the Prediction of Cardiovascular Disease and Diabetes: 0·5 Could Be a Suitable Global Boundary Value. Nutr. Res. Rev. 2010, 23, 247–269. [Google Scholar] [CrossRef]
- Lohman, T.G. The Use of Skinfold to Estimate Body Fatness on Children and Youth. J. Phys. Educ. Recreat. Danc. 1987, 58, 98–103. [Google Scholar] [CrossRef]
- Currie, C.; Molcho, M.; Boyce, W.; Holstein, B.; Torsheim, T.; Richter, M. Researching Health Inequalities in Adolescents: The Development of the Health Behaviour in School-Aged Children (HBSC) Family Affluence Scale. Soc. Sci. Med. 2008, 66, 1429–1436. [Google Scholar] [CrossRef]
- Cabanas-Sánchez, V.; Tejero-González, C.M.; Veiga, O.L. Construction and validation of a short scale of perception of barriers for the physical activity in adolescents. Rev. Esp. Salud Publica 2012, 86, 435–443. [Google Scholar] [CrossRef]
- Saint-Maurice, P.F.; Welk, G.J.; Beyler, N.K.; Bartee, R.T.; Heelan, K.A. Calibration of Self-Report Tools for Physical Activity Research: The Physical Activity Questionnaire (PAQ). BMC Public Health 2014, 14, 461. [Google Scholar] [CrossRef]
- Reimers, A.K.; Jekauc, D.; Mess, F.; Mewes, N.; Woll, A. Validity and Reliability of a Self-Report Instrument to Assess Social Support and Physical Environmental Correlates of Physical Activity in Adolescents. BMC Public Health 2012, 12, 705. [Google Scholar] [CrossRef]
- Grao-Cruces, A. Influencia de Padres y Amigos Sobre La Actividad Física de Tiempo Libre En Escolares Españoles de 12–16 Años: Diferencias Por Sexo e Intensidad. Nutr. Hosp. 2016, 33. [Google Scholar] [CrossRef]
- Wenden, E.J.; Lester, L.; Zubrick, S.R.; Ng, M.; Christian, H.E. The Relationship between Dog Ownership, Dog Play, Family Dog Walking, and Pre-Schooler Social–Emotional Development: Findings from the PLAYCE Observational Study. Pediatr. Res. 2021, 89, 1013–1019. [Google Scholar] [CrossRef] [PubMed]
- Brown, B.B.; Jensen, W.A. Dog Ownership and Walking: Perceived and Audited Walkability and Activity Correlates. Int. J. Environ. Res. Public Health 2020, 17, 1385. [Google Scholar] [CrossRef] [PubMed]
- Quante, M.; Kaplan, E.R.; Rueschman, M.; Cailler, M.; Buxton, O.M.; Redline, S. Practical Considerations in Using Accelerometers to Assess Physical Activity, Sedentary Behavior, and Sleep. Sleep Health 2015, 1, 275–284. [Google Scholar] [CrossRef] [PubMed]
- Trost, S.G.; Mciver, K.L.; Pate, R.R. Conducting Accelerometer-Based Activity Assessments in Field-Based Research. Med. Sci. Sports Exerc. 2005, 37, S531–S543. [Google Scholar] [CrossRef] [PubMed]
- Saint-Maurice, P.F.; Welk, G.J. Validity and Calibration of the Youth Activity Profile. PLoS ONE 2015, 10, e0143949. [Google Scholar] [CrossRef] [PubMed]
- Segura-Díaz, J.M.; Barranco-Ruiz, Y.; Saucedo-Araujo, R.G.; Aranda-Balboa, M.J.; Cadenas-Sanchez, C.; Migueles, J.H.; Saint-Maurice, P.F.; Ortega, F.B.; Welk, G.J.; Herrador-Colmenero, M.; et al. Feasibility and Reliability of the Spanish Version of the Youth Activity Profile Questionnaire (YAP-Spain) in Children and Adolescents. J. Sports Sci. 2021, 39, 801–807. [Google Scholar] [CrossRef]
- Saint-Maurice, P.F.; Kim, Y.; Hibbing, P.; Oh, A.Y.; Perna, F.M.; Welk, G.J. Calibration and Validation of the Youth Activity Profile: The FLASHE Study. Am. J. Prev. Med. 2017, 52, 880–887. [Google Scholar] [CrossRef]
- Bull, F.C.; Al-Ansari, S.S.; Biddle, S.; Borodulin, K.; Buman, M.P.; Cardon, G.; Carty, C.; Chaput, J.-P.; Chastin, S.; Chou, R.; et al. World Health Organization 2020 Guidelines on Physical Activity and Sedentary Behaviour. Br. J. Sports Med. 2020, 54, 1451–1462. [Google Scholar] [CrossRef]
- Hirshkowitz, M.; Whiton, K.; Albert, S.M.; Alessi, C.; Bruni, O.; DonCarlos, L.; Hazen, N.; Herman, J.; Adams Hillard, P.J.; Katz, E.S.; et al. National Sleep Foundation’s Updated Sleep Duration Recommendations: Final Report. Sleep Health 2015, 1, 233–243. [Google Scholar] [CrossRef]
- Chillón, P.; Herrador-Colmenero, M.; Migueles, J.H.; Cabanas-Sánchez, V.; Fernández-Santos, J.R.; Veiga, Ó.L.; Castro-Piñero, J.; Marcos, A.; Marcos, A.; Veiga, O.L.; et al. Convergent Validation of a Questionnaire to Assess the Mode and Frequency of Commuting to and from School. Scand. J. Public Health 2017, 45, 612–620. [Google Scholar] [CrossRef]
- Whitehead, M. Physical Literacy: Throughout the Lifecourse, 1st ed.; Whitehead, M., Ed.; International studies in physical education and youth sport; Routledge: London, UK; New York, NY, USA, 2010; ISBN 978-0-415-48742-9. [Google Scholar]
- Sum, R.K.W.; Ha, A.S.C.; Cheng, C.F.; Chung, P.K.; Yiu, K.T.C.; Kuo, C.C.; Yu, C.K.; Wang, F.J. Construction and Validation of a Perceived Physical Literacy Instrument for Physical Education Teachers. PLoS ONE 2016, 11, e0155610. [Google Scholar] [CrossRef] [PubMed]
- Sum, R.K.W.; Cheng, C.-F.; Wallhead, T.; Kuo, C.-C.; Wang, F.-J.; Choi, S.-M. Perceived Physical Literacy Instrument for Adolescents: A Further Validation of PPLI. J. Exerc. Sci. Fit. 2018, 16, 26–31. [Google Scholar] [CrossRef] [PubMed]
- Beaton, D.E.; Bombardier, C.; Guillemin, F.; Ferraz, M.B. Guidelines for the Process of Cross-Cultural Adaptation of Self-Report Measures. Spine 2000, 25, 3186–3191. [Google Scholar] [CrossRef] [PubMed]
- Harvey, A.; Faulkner, G.; Giangregorio, L.; Leatherdale, S.T. An Examination of School- and Student-Level Characteristics Associated with the Likelihood of Students’ Meeting the Canadian Physical Activity Guidelines in the COMPASS Study. Can. J. Public Health 2017, 108, 348–354. [Google Scholar] [CrossRef]
- Xin, F.; Zhu, Z.; Chen, S.; Chen, H.; Hu, X.; Ma, X.; Liang, K.; Liu, Y.; Wang, L.; Cai, Y.; et al. Prevalence and Correlates of Meeting the Muscle-Strengthening Exercise Recommendations among Chinese Children and Adolescents: Results from 2019 Physical Activity and Fitness in China—The Youth Study. J. Sport Health Sci. 2021, S2095254621001071. [Google Scholar] [CrossRef]
- Merlo, C.L.; Jones, S.E.; Michael, S.L.; Chen, T.J.; Sliwa, S.A.; Lee, S.H.; Brener, N.D.; Lee, S.M.; Park, S. Dietary and Physical Activity Behaviors Among High School Students—Youth Risk Behavior Survey, United States, 2019. MMWR Suppl. 2020, 69, 64–76. [Google Scholar] [CrossRef]
- Smith, J.J.; Diallo, T.M.O.; Bennie, J.A.; Tomkinson, G.R.; Lubans, D.R. Factors Associated with Adherence to the Muscle-Strengthening Activity Guideline among Adolescents. Psychol. Sport Exerc. 2020, 51, 101747. [Google Scholar] [CrossRef]
- Roth, S.E.; Gill, M.; Chan-Golston, A.M.; Rice, L.N.; Crespi, C.M.; Koniak-Griffin, D.; Cole, B.L.; Upchurch, D.M.; Prelip, M.L. Physical Activity Correlates in Middle School Adolescents: Perceived Benefits and Barriers and Their Determinants. J. Sch. Nurs. 2019, 35, 348–358. [Google Scholar] [CrossRef]
- Morrow, J.R.; Tucker, J.S.; Jackson, A.W.; Martin, S.B.; Greenleaf, C.A.; Petrie, T.A. Meeting Physical Activity Guidelines and Health-Related Fitness in Youth. Am. J. Prev. Med. 2013, 44, 439–444. [Google Scholar] [CrossRef]
- Casas, F.; Madorell, L. Preferències i Expectatives dels Adolescents Relatives a la Televisiò a Catalunya; Consell de l’Audiovisual de Catalunya: Barcelona, Spain, 2007; ISBN 978-84-393-7494-7. [Google Scholar]
- Serra-Majem, L.; Ribas, L.; Ngo, J.; Ortega, R.M.; García, A.; Pérez-Rodrigo, C.; Aranceta, J. Food, Youth and the Mediterranean Diet in Spain. Development of KIDMED, Mediterranean Diet Quality Index in Children and Adolescents. Public Health Nutr. 2004, 7, 931–935. [Google Scholar] [CrossRef]
- García-Hermoso, A.; Ezzatvar, Y.; López-Gil, J.F.; Ramírez-Vélez, R.; Olloquequi, J.; Izquierdo, M. Is Adherence to the Mediterranean Diet Associated with Healthy Habits and Physical Fitness? A Systematic Review and Meta-Analysis Including 565,421 Youths. Br. J. Nutr. 2020, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Rodríguez, I.T.; Ballart, J.F.; Pastor, G.C.; Jordà, E.B.; Val, V.A. Validation of a short questionnaire on frequency of dietary intake: Reproducibility and validity. Nutr. Hosp. 2008, 23, 242–252. [Google Scholar] [PubMed]
- Aranceta-Bartrina, J.; Partearroyo, T.; López-Sobaler, A.M.; Ortega, R.M.; Varela-Moreiras, G.; Serra-Majem, L.; Pérez-Rodrigo, C.; The Collaborative Group for the Dietary Guidelines for the Spanish Population (SENC). Updating the Food-Based Dietary Guidelines for the Spanish Population: The Spanish Society of Community Nutrition (SENC) Proposal. Nutrients 2019, 11, 2675. [Google Scholar] [CrossRef] [PubMed]
- Tanofsky-Kraff, M.; Theim, K.R.; Yanovski, S.Z.; Bassett, A.M.; Burns, N.P.; Ranzenhofer, L.M.; Glasofer, D.R.; Yanovski, J.A. Validation of the Emotional Eating Scale Adapted for Use in Children and Adolescents (EES-C). Int. J. Eat. Disord. 2007, 40, 232–240. [Google Scholar] [CrossRef]
- Perpiñá, C.; Cebolla, A.; Botella, C.; Lurbe, E.; Torró, M.-I. Emotional Eating Scale for Children and Adolescents: Psychometric Characteristics in a Spanish Sample. J. Clin. Child Adolesc. Psychol. 2011, 40, 424–433. [Google Scholar] [CrossRef]
- Shankar-Krishnan, N.; Penelo, E.; Fornieles Deu, A.; Sánchez-Carracedo, D. Spanish Adaptation and Validation of the Child Food Security Survey Module (CFSSM-S). Public Health Nutr. 2018, 21, 2753–2761. [Google Scholar] [CrossRef]
- Connell, C.L.; Nord, M.; Lofton, K.L.; Yadrick, K. Food Security of Older Children Can Be Assessed Using a Standardized Survey Instrument. J. Nutr. 2004, 134, 2566–2572. [Google Scholar] [CrossRef]
- US Department of Agriculture, Economic Research Service. Household Food Security in the United States in 2020; USDA: Washington, DC, USA, 2021.
- Larson, N.I.; Neumark-Sztainer, D.; Hannan, P.J.; Story, M. Family Meals during Adolescence Are Associated with Higher Diet Quality and Healthful Meal Patterns during Young Adulthood. J. Am. Diet. Assoc. 2007, 107, 1502–1510. [Google Scholar] [CrossRef]
- Neumark-Sztainer, D.; Eisenberg, M.E.; Fulkerson, J.A.; Story, M.; Larson, N.I. Family Meals and Disordered Eating in Adolescents: Longitudinal Findings From Project EAT. Arch. Pediatr. Adolesc. Med. 2008, 162, 17. [Google Scholar] [CrossRef]
- Larson, N.I.; Nelson, M.C.; Neumark-Sztainer, D.; Story, M.; Hannan, P.J. Making Time for Meals: Meal Structure and Associations with Dietary Intake in Young Adults. J. Am. Diet. Assoc. 2009, 109, 72–79. [Google Scholar] [CrossRef]
- Neumark-Sztainer, D.; Wall, M.; Guo, J.; Story, M.; Haines, J.; Eisenberg, M. Obesity, Disordered Eating, and Eating Disorders in a Longitudinal Study of Adolescents: How Do Dieters Fare 5 Years Later? J. Am. Diet. Assoc. 2006, 106, 559–568. [Google Scholar] [CrossRef] [PubMed]
- Neumark-Sztainer, D.; Story, M.; Hannan, P.J.; Perry, C.L.; Irving, L.M. Weight-Related Concerns and Behaviors Among Overweight and Nonoverweight Adolescents: Implications for Preventing Weight-Related Disorders. Arch. Pediatr. Adolesc. Med. 2002, 156, 171. [Google Scholar] [CrossRef] [PubMed]
- Garaulet, M.; Madrid, J.A. Métodos Cronobiológicos En Las Encuestas Alimentarias: Criterios de Aplicación e Interpretación De. Nutr. Hosp. 2015, 279–289. [Google Scholar] [CrossRef]
- Martínez-Lozano, N.; Tvarijonaviciute, A.; Ríos, R.; Barón, I.; Scheer, F.A.J.L.; Garaulet, M. Late Eating Is Associated with Obesity, Inflammatory Markers and Circadian-Related Disturbances in School-Aged Children. Nutrients 2020, 12, 2881. [Google Scholar] [CrossRef] [PubMed]
- Larson, N.I.; Story, M.; Eisenberg, M.E.; Neumark-Sztainer, D. Food Preparation and Purchasing Roles among Adolescents: Associations with Sociodemographic Characteristics and Diet Quality. J. Am. Diet. Assoc. 2006, 106, 211–218. [Google Scholar] [CrossRef]
- Larson, N.; Laska, M.N.; Neumark-Sztainer, D. Do Young Adults Value Sustainable Diet Practices? Continuity in Values from Adolescence to Adulthood and Linkages to Dietary Behaviour. Public Health Nutr. 2019, 22, 2598–2608. [Google Scholar] [CrossRef]
- Roberts, C.; Freeman, J.; Samdal, O.; Schnohr, C.W.; de Looze, M.E.; Nic Gabhainn, S.; Iannotti, R.; Rasmussen, M.; the International HBSC Study Group. The Health Behaviour in School-Aged Children (HBSC) Study: Methodological Developments and Current Tensions. Int. J. Public Health 2009, 54, 140–150. [Google Scholar] [CrossRef]
- Davies, R.M.; Davies, G.M.; Ellwood, R.P.; Kay, E.J. Prevention. Part 4: Toothbrushing: What Advice Should Be given to Patients? Br. Dent. J. 2003, 195, 135–141. [Google Scholar] [CrossRef]
- Iannotti, R.J.; Janssen, I.; Haug, E.; Kololo, H.; Annaheim, B.; Borraccino, A.; the HBSC Physical Activity Focus Group. Interrelationships of Adolescent Physical Activity, Screen-Based Sedentary Behaviour, and Social and Psychological Health. Int. J. Public Health 2009, 54, 191–198. [Google Scholar] [CrossRef]
- Zaborskis, A.; Sumskas, L.; Maser, M.; Pudule, I. Trends in Drinking Habits among Adolescents in the Baltic Countries over the Period of Transition: HBSC Survey Results, 1993–2002. BMC Public Health 2006, 6, 67. [Google Scholar] [CrossRef][Green Version]
- Currie, C.; Hurrelmann, K.; Settertobulte, W.; Smith, R.; Todd, J. Health and Health Behaviour among Young People; WHO: Geneva, Switzerland, 2000. [Google Scholar]
- Ruiz, J.R.; Castro-Pinero, J.; Espana-Romero, V.; Artero, E.G.; Ortega, F.B.; Cuenca, M.M.; Jimenez-Pavon, D.; Chillon, P.; Girela-Rejon, M.J.; Mora, J.; et al. Field-Based Fitness Assessment in Young People: The ALPHA Health-Related Fitness Test Battery for Children and Adolescents. Br. J. Sports Med. 2011, 45, 518–524. [Google Scholar] [CrossRef] [PubMed]
- Ortega, F.B.; Artero, E.G.; Ruiz, J.R.; Espana-Romero, V.; Jimenez-Pavon, D.; Vicente-Rodriguez, G.; Moreno, L.A.; Manios, Y.; Beghin, L.; Ottevaere, C.; et al. Physical Fitness Levels among European Adolescents: The HELENA Study. Br. J. Sports Med. 2011, 45, 20–29. [Google Scholar] [CrossRef] [PubMed]
- Castro-Piñero, J.; Chillón, P.; Ortega, F.B.; Montesinos, J.L.; Sjöström, M.; Ruiz, J.R. Criterion-Related Validity of Sit-and-Reach and Modified Sit-and-Reach Test for Estimating Hamstring Flexibility in Children and Adolescents Aged 6–17 Years. Int. J. Sports Med. 2009, 30, 658–662. [Google Scholar] [CrossRef] [PubMed]
- Ortega, F.B.; Ruiz, J.R.; España-Romero, V.; Vicente-Rodriguez, G.; Martínez-Gómez, D.; Manios, Y.; Béghin, L.; Molnar, D.; Widhalm, K.; Moreno, L.A.; et al. The International Fitness Scale (IFIS): Usefulness of Self-Reported Fitness in Youth. Int. J. Epidemiol. 2011, 40, 701–711. [Google Scholar] [CrossRef]
- Lurbe, E.; Agabiti-Rosei, E.; Cruickshank, J.K.; Dominiczak, A.; Erdine, S.; Hirth, A.; Invitti, C.; Litwin, M.; Mancia, G.; Pall, D.; et al. 2016 European Society of Hypertension Guidelines for the Management of High Blood Pressure in Children and Adolescents. J. Hypertens. 2016, 34, 1887–1920. [Google Scholar] [CrossRef]
- Owens, J.A.; Dalzell, V. Use of the ‘BEARS’ Sleep Screening Tool in a Pediatric Residents’ Continuity Clinic: A Pilot Study. Sleep Med. 2005, 6, 63–69. [Google Scholar] [CrossRef]
- Bastida-Pozuelo, M.F.; Sánchez-Ortuño, M.M. Preliminary Analysis of the Concurrent Validity of the Spanish Translation of the BEARS Sleep Screening Tool for Children. J. Psychiatr. Ment. Health Nurs. 2016, 23, 513–520. [Google Scholar] [CrossRef]
- Carskadon, M.A.; Vieira, C.; Acebo, C. Association between Puberty and Delayed Phase Preference. Sleep 1993, 16, 258–262. [Google Scholar] [CrossRef]
- Díaz-Morales, J.F.; de León, M.C.D.; Sorroche, M.G. Validity of the Morningness-Eveningness Scale for Children among Spanish Adolescents. Chronobiol. Int. 2007, 24, 435–447. [Google Scholar] [CrossRef]
- Tanner, J.M. 1 Normal Growth and Techniques of Growth Assessment. Clin. Endocrinol. Metab. 1986, 15, 411–451. [Google Scholar] [CrossRef]
- Tapia-Serrano, M.A.; Esteban-Cornejo, I.; Rodriguez-Ayllon, M.; Vaquero-Solís, M.; Sánchez-Oliva, D.; Sánchez-Miguel, P.A. Adherence to the Mediterranean Diet and Academic Performance in Adolescents: Does BMI Status Moderate This Association? Clin. Nutr. 2021, 40, 4465–4472. [Google Scholar] [CrossRef] [PubMed]
- Muntaner-Mas, A.; Martínez-Gómez, D.; Castro- Piñero, J.; Fernandez-Santos, J.R.; Salmon, J.; Veiga, Ó.L.; Esteban-Cornejo, I. Objectively Measured Physical Activity and Academic Performance in School-aged Youth: The UP&DOWN Longitudinal Study. Scand. J. Med. Sci. Sports 2021, 31, 2230–2240. [Google Scholar] [CrossRef] [PubMed]
- Martinez-Zamora, M.D.; Valenzuela, P.L.; Pinto-Escalona, T.; Martinez-de-Quel, Ó. The “Fat but Fit” Paradox in the Academic Context: Relationship between Physical Fitness and Weight Status with Adolescents’ Academic Achievement. Int. J. Obes. 2021, 45, 95–98. [Google Scholar] [CrossRef]
- Garcia-Campayo, J.; Sanz-Carrillo, C.; Ibañez, J.A.; Lou, S.; Solano, V.; Alda, M. Validation of the Spanish Version of the SCOFF Questionnaire for the Screening of Eating Disorders in Primary Care. J. Psychosom. Res. 2005, 59, 51–55. [Google Scholar] [CrossRef]
- Segura-García, C.; Papaianni, M.C.; Rizza, P.; Flora, S.; De Fazio, P. The Development and Validation of the Body Image Dimensional Assessment (BIDA). Eat. Weight. Disord. Stud. Anorex. Bulim. Obes. 2012, 17. [Google Scholar] [CrossRef]
- Sánchez-Miguel, P.A.; Vaquero-Solís, M.; Sánchez-Oliva, D.; Pulido-González, J.J.; Segura-García, C.; Tapia-Serrano, M.A. Validation of the Body Image Dimensional Assessment in Adolescents from Spanish High School. Eat. Weight Disord. 2021, 26, 1749–1756. [Google Scholar] [CrossRef]
- Ravens-Sieberer, U. The KIDSCREEN Questionnaires: Quality of Life Questionnaires for Children and Adolescents; The KIDSCREEN questionnaires: Quality of life questionnaires for children and adolescents; Pabst Science Publishers: Lengerich, Germany, 2006; p. 231. ISBN 978-3-89967-334-0. [Google Scholar]
- Aymerich, M.; Berra, S.; Guillamón, I.; Herdman, M.; Alonso, J.; Ravens-Sieberer, U.; Rajmil, L. Desarrollo de la versión en español del KIDSCREEN, un cuestionario de calidad de vida para la población infantil y adolescente. Gac. Sanit. 2005, 19, 93–102. [Google Scholar] [CrossRef]
- Rosenberg, M. Society and the Adolescent Self-Image; Princeton Legacy Library; Princeton University Press: Princeton, NJ, USA, 2016; ISBN 978-1-4008-7613-6. [Google Scholar]
- Martín-Albo, J.; Núñez, J.L.; Navarro, J.G.; Grijalvo, F. The Rosenberg Self-Esteem Scale: Translation and Validation in University Students. Span. J. Psychol. 2007, 10, 458–467. [Google Scholar] [CrossRef]
- Pichardo, M.C.; Cano, F.; Garzón-Umerenkova, A.; de la Fuente, J.; Peralta-Sánchez, F.J.; Amate-Romera, J. Self-Regulation Questionnaire (SRQ) in Spanish Adolescents: Factor Structure and Rasch Analysis. Front. Psychol. 2018, 9, 1370. [Google Scholar] [CrossRef]
- Brown, J.M.; Miller, W.R.; Lawendowski, L.A. The Self-Regulation Questionnaire. In Innovations in Clinical Practice: A Source Book, Vol. 17; Professional Resource Press/Professional Resource Exchange: Sarasota, FL, USA, 1999; pp. 281–292. ISBN 1-56887-049-3. [Google Scholar]
- Pichardo, C.; Justicia, F.; de la Fuente, J.; Martínez-Vicente, J.M.; Berbén, A.B.G. Factor Structure of the Self-Regulation Questionnaire (SRQ) at Spanish Universities. Span. J. Psychol. 2014, 17, E62. [Google Scholar] [CrossRef]
- Baessler, J.; Schwarzer, R. Evaluación de La Autoeficacia: Adaptación Española de La Escala de Autoeficacia General. Measuring Optimistic Self-Beliefs: A Spanish Adaptation of the General Self-Efficacy Scale. Ansiedad Estrés 1996, 2, 1–8. [Google Scholar]
- Espada, J.P.; Gonzálvez, M.T.; Orgilés, M.; Carballo, J.L.; Piqueras, J.A. Validación de La Escala de Autoeficacia General Con Adolescentes Españoles. EJREP 2017, 10, 355–370. [Google Scholar] [CrossRef]
- Schwarzer, R.; Freie Universitat Berlin. Measurement of Perceived Self-Efficacy: Psychometric Scales for Cross-Cultural Research; Freien Universitat: Berlin, Germany, 1993; ISBN 978-3-927433-24-3. [Google Scholar]
- Sanjuán Suárez, P.; Pérez García, A.M.; Bermúdez Moreno, J. Escala de Autoeficacia General: Datos Psicométricos de La Adaptación Para Población Española. Psicothema 2000, 12, 509–513. [Google Scholar]
- Goodman, R. The Strengths and Difficulties Questionnaire: A Research Note. J. Child Psychol. Psychiatry 1997, 38, 581–586. [Google Scholar] [CrossRef]
- Ezpeleta, L.; Granero, R.; de la Osa, N.; Penelo, E.; Domènech, J.M. Psychometric Properties of the Strengths and Difficulties Questionnaire3–4 in 3-Year-Old Preschoolers. Compr. Psychiatry 2013, 54, 282–291. [Google Scholar] [CrossRef]
- Ortuño-Sierra, J.; Fonseca-Pedrero, E.; Paíno, M.; Aritio-Solana, R. Prevalencia de síntomas emocionales y comportamentales en adolescentes españoles. Rev. Psiquiatr. Salud Ment. 2014, 7, 121–130. [Google Scholar] [CrossRef]
- Diener, E.; Emmons, R.A.; Larsen, R.J.; Griffin, S. The Satisfaction With Life Scale. J. Personal. Assess. 1985, 49, 71–75. [Google Scholar] [CrossRef]
- Vázquez, C.; Duque, A.; Hervás, G. Satisfaction with Life Scale in a Representative Sample of Spanish Adults: Validation and Normative Data. Span. J. Psychol. 2013, 16, E82. [Google Scholar] [CrossRef]
- Pavot, W.; Diener, E. The Affective and Cognitive Context of Self-Reported Measures of Subjective Well-Being. Soc. Indic. Res. 1993, 28, 1–20. [Google Scholar] [CrossRef]
- Ebesutani, C.; Regan, J.; Smith, A.; Reise, S.; Higa-McMillan, C.; Chorpita, B.F. The 10-Item Positive and Negative Affect Schedule for Children, Child and Parent Shortened Versions: Application of Item Response Theory for More Efficient Assessment. J. Psychopathol. Behav. Assess. 2012, 34, 191–203. [Google Scholar] [CrossRef]
- Damásio, B.F.; Pacico, J.C.; Poletto, M.; Koller, S.H. Refinement and Psychometric Properties of the Eight-Item Brazilian Positive and Negative Affective Schedule for Children (PANAS-C8). J. Happiness Stud. 2013, 14, 1363–1378. [Google Scholar] [CrossRef]
- Brighi, A.; Ortega, R.; Scheitauer, H.; Smith, P.K.; Tsormpatzoudis, C.; Barkoukis, V.; Del Rey, R.; Thompson, F. European Bullying Intervention Project Questionnaire (EBIPQ) (Unpublished Questionnaire); Univerity of Bolonia: Bolonia, Italy, 2012. [Google Scholar]
- Brighi, A.; Ortega, R.; Scheitauer, H.; Smith, P.K.; Tsormpatzoudis, C.; Barkoukis, V.; Del Rey, R.; Guarini, A.; Plichta, P.; Schultze-Krumbholz, A.; et al. European Cyberbullying Intervention Project Questionnaire (ECIPQ) (Unpublished Questionnaire); Univerity of Bolonia: Bolonia, Italy, 2012. [Google Scholar]
- Ortega-Ruiz, R.; Del Rey, R.; Casas, J.A. Evaluar el bullying y el cyberbullying validación española del EBIP-Q y del ECIP-Q. Psicol. Educ. 2016, 22, 71–79. [Google Scholar] [CrossRef]
- Developmental Studies Center. Youth Outcome Measures for AfterSchool KidzLitTM Evaluation—Subscale “Positive Behavior”; Developmental Studies Center: Alameda, CA, USA, 2001. [Google Scholar]
- Miranda, R.; Oriol, X.; Amutio, A.; Ortúzar, H. Adolescent Bullying Victimization and Life Satisfaction: Can Family and School Adult Support Figures Mitigate This Effect? Rev. Psicodidáctica (Engl. Ed.) 2019, 24, 39–45. [Google Scholar] [CrossRef]
- Lovibond, P.F.; Lovibond, S.H. The Structure of Negative Emotional States: Comparison of the Depression Anxiety Stress Scales (DASS) with the Beck Depression and Anxiety Inventories. Behav. Res. Ther. 1995, 33, 335–343. [Google Scholar] [CrossRef]
- Bados, A.; Solanas, A.; Andrés, R. Psychometric Properties of the Spanish Version of Depression, Anxiety and Stress Scales (DASS). Propiedades Psicométricas de La Versión Española de Las Escalas de Depresión, Ansiedad y Estrés (DASS). Psicothema 2005, 17, 679–683. [Google Scholar]
- Román, F.; Santibáñez, P.; Vinet, E.V. Uso de las Escalas de Depresión Ansiedad Estrés (DASS-21) como Instrumento de Tamizaje en Jóvenes con Problemas Clínicos. Acta Investig. Psicol. 2016, 6, 2325–2336. [Google Scholar] [CrossRef]
- Bond, F.W.; Hayes, S.C.; Baer, R.A.; Carpenter, K.M.; Guenole, N.; Orcutt, H.K.; Waltz, T.; Zettle, R.D. Preliminary Psychometric Properties of the Acceptance and Action Questionnaire–II: A Revised Measure of Psychological Inflexibility and Experiential Avoidance. Behav. Ther. 2011, 42, 676–688. [Google Scholar] [CrossRef]
- Ruiz, F.J.; Langer Herrera, Á.I.; Luciano, C. Measuring Experiential Avoidance and Psychological Inflexibility: The Spanish Version of the Acceptance and Action Questionnaire-II. Psicothema 2013, 123–129. [Google Scholar] [CrossRef]
- Cuadrado, E.; Rojas, R.; Tabernero, C. Development and Validation of the Social Network Addiction Scale (SNAddS-6S). Eur. J. Investig. Health Psychol. Educ. 2020, 10, 763–778. [Google Scholar] [CrossRef]
- Estudio ALADINO 2019. Estudio de Vigilancia Del Crecimiento, Alimentación, Actividad Física, Desarrollo Infantil y Obesidad En España 2019; Ministerio de Sanidad, Servicios Sociales e Igualdad: Madrid, Spain, 2020. [Google Scholar]
- Gasol Foundation. Resultados Principales Del Estudio PASOS 2019 Sobre La Actividad Física, Los Estilos de Vida y La Obesidad de La Población Española de 8 a 16 Años; Gasol Foundation: Barcelona, Spain, 2019. [Google Scholar]
- Gorber, S.C.; Tremblay, M.; Moher, D.; Gorber, B. A Comparison of Direct vs. Self-Report Measures for Assessing Height, Weight and Body Mass Index: A Systematic Review. Obes. Rev. 2007, 8, 307–326. [Google Scholar] [CrossRef]
- Tukuitonga, C.; Keller, I. Implementing the World Health Organization Global Strategy on Diet, Physical Activity and Health. Scand. J. Nutr. 2005, 49, 122–126. [Google Scholar] [CrossRef]
- Tremblay, M.S.; Gray, C.E.; Akinroye, K.; Harrington, D.M.; Katzmarzyk, P.T.; Lambert, E.V.; Liukkonen, J.; Maddison, R.; Ocansey, R.T.; Onywera, V.O.; et al. Physical Activity of Children: A Global Matrix of Grades Comparing 15 Countries. J. Phys. Act. Health 2014, 11, S113–S125. [Google Scholar] [CrossRef] [PubMed]
- Aubert, S.; Barnes, J.D.; Abdeta, C.; Abi Nader, P.; Adeniyi, A.F.; Aguilar-Farias, N.; Andrade Tenesaca, D.S.; Bhawra, J.; Brazo-Sayavera, J.; Cardon, G.; et al. Global Matrix 3.0 Physical Activity Report Card Grades for Children and Youth: Results and Analysis From 49 Countries. J. Phys. Act. Health 2018, 15, S251–S273. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
López-Gil, J.F. The Eating Healthy and Daily Life Activities (EHDLA) Study. Children 2022, 9, 370. https://doi.org/10.3390/children9030370
López-Gil JF. The Eating Healthy and Daily Life Activities (EHDLA) Study. Children. 2022; 9(3):370. https://doi.org/10.3390/children9030370
Chicago/Turabian StyleLópez-Gil, José Francisco. 2022. "The Eating Healthy and Daily Life Activities (EHDLA) Study" Children 9, no. 3: 370. https://doi.org/10.3390/children9030370
APA StyleLópez-Gil, J. F. (2022). The Eating Healthy and Daily Life Activities (EHDLA) Study. Children, 9(3), 370. https://doi.org/10.3390/children9030370





